Access: The TAC Blog
September 2019: Olmstead at 20 — Using the Vision of Olmstead to Decriminalize Mental Illness
June 22, 2019 marked the twentieth anniversary of the United States Supreme Court’s Olmstead v. L.C. decision. The case was filed on behalf of two women with developmental disabilities and mental illness who were confined in a state psychiatric hospital in Georgia despite their treatment professionals’ recommendations that they could live in the community. In its decision, the court stated that unjustified segregation of persons with disabilities constitutes discrimination in violation of Title II of the Americans with Disabilities Act (ADA). The ADA established a mandate to public entities to ensure that people with disabilities live in the least restrictive, most integrated settings possible.
Because of the Olmstead decision 20 years ago, many states have implemented policies, programs, and new housing options to serve people in the most integrated settings appropriate to their needs. Olmstead-based lawsuits and settlement agreements in several states have forced new resources and opportunities for community integration into both state and local systems. While such progress has been slow, an increase in attention to individuals with mental illness and other disabilities who are unnecessarily segregated — or at risk of becoming so — in settings such as psychiatric hospitals, nursing homes, and large board and care facilities has resulted in many more people with mental illness living in integrated, community-based settings.
Yet for far too many people with mental illness who end up unnecessarily in another type of segregated setting — jails and prisons — the promise of the ADA and the Olmstead decision remains unfulfilled. The incarceration of people with mental illness in communities throughout the United States is a form of discrimination that our public entities must address.
In March 2019, TAC convened top thinkers from across the U.S. to examine the criminalization of persons with mental illness, and to initiate the use of Olmstead as a framework for reform. Based on insights from that group, TAC has prepared and published Olmstead at 20: Expanding the Vision of Olmstead to Decriminalize Mental Illness. In this brief, we apply key elements of Olmstead law to the challenge of reducing the disproportionate number of people with mental illness in the criminal justice system.
Segregated Settings and the Integration Mandate
Understanding how Olmstead applies to the correctional system begins with recognizing that jails and prisons are institutions and that the U.S. Department of Justice’s definition of “segregated settings” applies to them. The “integration mandate” is a fundamental aspect of the ADA, requiring public entities to “administer services, programs, and activities in the most integrated setting appropriate to the needs of qualified individuals with disabilities.” For most individuals, receiving services in the community is the most integrated setting, and an absence of such services, leading to institutionalization, reflects a violation of the ADA. Many individuals with mental illness in correctional settings are there because community-based services and settings were not available to meet their needs — even as public funding is used to sustain the costs of housing people in the segregated correctional system.
Community-Based Services Play a Vital Role
Underdeveloped service delivery systems, budget cuts, loss of insurance coverage, and tightened program eligibility requirements not only reduce people’s access to community services, but also make it harder for them to pay for medication, treatment, and housing. When people with mental illness lack access to comprehensive, community-based treatment and support services, they are at greater risk of ending up in institutional, segregated settings, including correctional facilities.
In service systems across the country, encounters between people with mental illness and law enforcement can be traced to a lack of community-based treatment and services. If there is no hotline, mobile crisis team, or mental health respite program, the only option for a person in crisis or their family may be to call the police — whose only option may be to arrest the person.
Taking the Next Steps
If you represent a public entity at any level, we encourage you to launch initiatives that minimize preventable interactions with the criminal justice system. Furthermore, such measures should be fully incorporated into the Olmstead planning efforts of your state or county to meet their legal obligations. We hope that other interested stakeholders, such as advocates and civil rights groups, will also find this framework of use for Olmstead planning and advocacy efforts.
December 2018: Permanent Supportive Housing — Renewing Our Commitment
Last week, I had the pleasure of delivering the keynote address at the annual conference of the Supportive Housing Association of New Jersey. This gathering marked the association’s 20th anniversary, an opportunity to reflect on two decades of work to make permanent supportive housing — i.e., lease-based housing paired with voluntary, flexible services — a primary intervention for people with a wide range of disabilities and for people experiencing or at risk of homelessness. Many other states, too, have invested time and resources in the successful expansion of this approach for their homeless and disabled populations.
In an interesting fluke of timing, the New York Times had published an article the day before the conference, highlighting negative stories about permanent supportive housing (PSH) in New York and painting a picture of a model that had too often failed persons with serious mental illness. The tone of the article was keenly felt by this group of PSH practitioners, and several leaders from other states and policy groups have since contacted me to discuss the article’s potential impact. How could PSH — an approach that leaders in many states are working to expand in order to support the community integration needs of those who are homeless or disabled — be represented as a failure? What are the article’s implications for those seeking to invest in or expand PSH, for providers, and for people determined to live independently?
While the Times article was alarming, strong evidence nevertheless suggests that people with serious mental illness can succeed in PSH, and that use of the model should indeed be expanded. But there are considerations that must be addressed to ensure that PSH meets the needs of the people it is intended to serve.
Supportive Housing Works
People with serious mental illness have historically lived in institutional settings whether they actually needed to or not. Over time, however, understanding has grown that the policy of housing people in state psychiatric hospitals, for example, is both cost-ineffective and inhumane, and that it fails to demonstrate positive outcomes. Deinstitutionalization efforts from the 1970s to the 1990s meant that many more people with mental illness began living in the community. We all know the story of the resulting growth in homelessness and trans-institutionalization to correctional settings, as public systems failed to develop their community-based services capacity and affordable housing resources to meet the increase in demand. Some people had access to services and residential supports, but many did not, and many still do not today.
When I was a case manager over 20 years ago, "supportive housing" meant doing everything possible to get people with mental illness into housing and helping them stay there. Over time, anecdotal stories of success across the country evolved into an evidence base for what we now know as permanent supportive housing.
There is plenty of evidence to demonstrate the effectiveness of PSH for people with mental illness and for people transitioning from homelessness. Many PSH programs have shown increased housing stability, decreased emergency department and inpatient use, reduced jail days, and significant cost savings compared to homelessness, inpatient care, and other institutional or supervised settings.
Even the statistics noted by the Times suggest that a large majority of people have succeeded in supportive housing. It is important to regard this in light of evidence showing safety and quality of care concerns in New York's adult homes, the housing situation from which many people with mental illness move into supportive housing.
Services Must Be Well-Designed and Adequately Funded
Does supportive housing work for everyone? No. Some people need supervised treatment settings, or prefer group residential programs. However, contrary to the assumptions that used to govern our mental health care systems, supportive housing in the community has been shown to work for a variety of people, including those with the most significant needs who are transitioning from state psychiatric hospitals, nursing facilities, jails, or homelessness. Even people with the most complex conditions need a place to call home that is not contingent on being a "compliant" patient or a "good" client; in fact, providing a choice of housing together with voluntary services has been shown to strengthen retention in housing and services.
In order for PSH to be successful, particularly for persons with complex needs, services must be voluntary, flexible, responsive, robust, and comprehensive. Furthermore, they must be delivered by well-trained staff who are able to provide the right types of services, in the right locations (i.e., where people live), and at the right times, adapting what is offered to meet individuals’ evolving needs. Providers that struggle to adequately support people in PSH are often those with inadequate staffing, which makes them unable to respond quickly and appropriately.
To underfund services is to undermine the ability of providers to meet the needs of PSH tenants. In my experience, the services covered by Medicaid are not, on their own, enough to meet the needs of many people who could otherwise succeed in PSH. If systems will be expected to serve an increasingly complex population, state and county funding agencies and Medicaid managed care organizations must have adequate resources available to pay for a full range of services; successful permanent supportive housing programs are those that braid or blend Medicaid with other resources.
Building On the Evidence
As a former state mental health commissioner, a behavioral health provider, and the family member of someone with a mental illness, it boggles my mind that we would rather pay several hundred thousand dollars per year to house a person in an institutional setting than commit a fraction of that amount to support them in an integrated, community-based setting with demonstrated positive outcomes. Too often, the response to challenges that arise in PSH is an assumption that a person is "not ready," or "needs supervision," instead of a person-centered mindset that tailors and continually adapts services to each individual’s needs and choices.
Yes, people with mental illness and other disabilities may need inpatient treatment, at times. They may need round-the-clock support, at times. They may need assistance with their medications, at times. They may need transportation to medical appointments, at times. People with mental illness and other disabilities may need lots of things — but that doesn’t mean we should return to institutionalization at a cost that is much greater than the sum required to meet all of those needs. With sufficient resources to pay for both rental assistance and robust, flexible services, permanent supportive housing can be a primary intervention for individuals with complex needs.
Systems should move forward on bringing well-designed, fully funded permanent supportive housing to scale, so that all who can benefit from living in safe, independent, community-integrated housing have the opportunity to do so.
November 2017: Putting Psychiatric Hospitalization into Context
THE NUMBER OF STATE INSTITUTIONAL PSYCHIATRIC BEDS, which were once the primary setting for psychiatric treatment, has gone down dramatically nationwide. Community psychiatric hospitals, private hospitals, and nursing facilities filled the gap in the 1980s and '90s, but inpatient capacity in these settings, too, has recently been on the decline. There is widespread concern — given ample voice by the media — that we need to restore our nation’s psychiatric bed capacity, both to reduce the risk of violence perpetrated by people with untreated mental illness, and for their own safety and health.
In reality, however, inpatient treatment should form only one part of a robust system of mental health care. For comparison, note that treatment for even the most serious medical conditions now frequently occurs in outpatient and in-home settings. However, recent findings from the Healthcare Cost and Utilization Project reveal a widening gap between our country’s approaches to hospitalization for mental and for physical health conditions: Between 2005 and 2014, the rate of inpatient stays per 100,000 people for all causes decreased across all age groups, while the number of hospital stays for mental health/substance use actually increased by 12.2 percent.
To examine these trends and their implications, the National Association of State Mental Health Program Directors recently commissioned a series of working papers on the question: “What is the real need for inpatient psychiatric beds in the context of a best practice continuum of care?” In this series, researchers and policy leaders describe ways to improve mental health and substance use disorder treatment at many different points in a community’s system of care so as to necessitate fewer psychiatric hospitalizations, of shorter duration, with better and more equitable outcomes.
Increasing the number of psychiatric inpatient beds is not the solution in most communities. As my colleague Kevin Martone and I argue in our contributions to the series, investments in care and services can create alternatives to inpatient beds that are both more effective and less costly. “Beyond Beds: The Vital Role of a Full Continuum of Psychiatric Care” lays out specific public policy recommendations to minimize the human and economic costs associated with severe mental illness by building and invigorating a robust, interconnected, and evidence-based system of care. And as “The Role of Permanent Supportive Housing in Determining Psychiatric Inpatient Bed Capacity” shows, stable and affordable housing combined with voluntary services can contribute to improved outcomes in both physical and behavioral health, while reducing incarceration and homelessness. Furthermore, the cost of serving a person in supportive housing is half that of a shelter, a quarter that of incarceration, and one-tenth the cost of a state psychiatric hospital bed.
Advances in medical research and technology, chronic disease management programs, and alternative treatment settings such as walk-in urgent care centers — along with payment approaches that support medical care in outpatient settings — have all helped reduce hospitalizations for physical health conditions. Evidence-based mental health care options, especially when provided in the communities where people live, offer the potential to bring down psychiatric hospitalizations as well. Private insurers rarely cover these services, however, and state and federal mental health funding are drastically insufficient to meet demand. Medicare and Medicaid together fund approximately 60 percent of inpatient care in the United States. Unfortunately, Medicare funds very few evidence-based mental health practices, and Medicaid funding for housing transition and tenancy-sustaining programs — a critical component of permanent supportive housing for people with mental health disabilities — is not yet fully incorporated into services.
We don’t need to re-create massive numbers of psychiatric inpatient beds. Rather, policymakers must prioritize funding for the evidence-based preventive treatment and services that people with mental illness need and desire. With these effective and cost-saving resources available and truly accessible in every community, hospitalization will play an appropriate role in a balanced system.
September 2017: News, Resources, & Happenings at TAC
“It Makes Me Feel Like I Mean Something”: Success Stories in Community Integration
Permanent supportive housing enables many people with disabilities to live independently and participate fully in their families and communities. The Section 811 Project Rental Assistance program of the Department of Housing and Urban Development (HUD) helps communities forge partnerships and leverage resources to help people move out of unnecessarily restrictive environments and into their own apartments - and to help them thrive once there. In these videos and vignettes produced by the HUD Office of Multifamily Housing with TAC's assistance, you'll see how community integration through supportive housing looks for Tanesha, Destiny, Avia, and Mr. Poole, four individuals with diverse needs and histories who live in different parts of the country. You will also hear from service providers and property managers about what makes the 811 PRA program work.
Determining the Real Need for Inpatient Psychiatric Beds
Two TAC authors have contributed working papers to a new series published by the National Association of State Mental Health Program Directors, taking on the question: "What is the inpatient bed need if you have a best practice continuum of care?" In The Role of Permanent Supportive Housing in Determining Psychiatric Inpatient Bed Capacity, Sherry Lerch and Kevin Martone discuss the importance of permanent supportive housing (PSH) as a core intervention in a strong community-based system, and how PSH capacity can reduce the demand for psychiatric inpatient beds. In The Role State Mental Health Authorities Can Play in the Delivery of Integrated Primary and Behavioral Health Care for People with Serious Mental Illness, Including Those with Co-Occurring Substance Use Disorders, Sherry Lerch lays out changes in planning, financing, and procedures that can help SMHAs improve care integration.
TAC Staff in Action
Staff Activities
TAC Managing Director Marie Herb and Senior Associate Liz Stewart both led workshops at the HOPWA Institute in Tampa, a HUD event focused on housing's role in ending the HIV epidemic; Associates Ashley Mann-McLellan and Douglas Tetrault and consultant Naomi Sweitzer helped design and deliver a series of intensive, day-long trainings for direct services staff in the Supportive Services for Veteran Families program; Executive Director Kevin Martone has been named to the board of the National Association for Rural Mental Health, and attended its annual conference in San Diego; Mayra Pabon, our Administrative Assistant, attended the Boston Center for Independent Living's celebration lunch for Transition Internship Program participants, including TAC summer intern Hawo Osman; Senior Consultant Lisa Sloane, Associate Ellen Fitzpatrick, and Production/Design Associate Adriana DePalma put the finishing touches on a series of "HUD PRA 811 Success Stories" which went live mid-month (see above); Senior Associate Jim Yates co-presented on "Supportive Services for Veteran Families and Beyond" at the Kansas Housing Conference; and Senior Associate Gina Schaak represented TAC at a "Massachusetts Housing Day" at the State House, organized by the Citizens' Housing and Planning Association.
Staff Transitions
We're happy to announce that Jennifer Ingle has joined TAC as an Associate with TAC's human services group. Jenn brings expertise in program evaluation, stakeholder engagement, and policy related to long-term services and supports, and has many years' experience working directly with elders and people with psychiatric disabilities. We are also delighted to welcome Madison Tallant, a graduate student in social work at Boston College, as a TAC intern with our housing team this year.
September 2017: Making a Healthier Workplace for Everyone
MANY PEOPLE WITH SERIOUS MENTAL HEALTH CONDITIONS (SMHCs) need employment income in order to meet their basic needs and live independently in the community. However, challenges both in finding and in keeping a job have kept unemployment and underemployment rates high in this group. “Supported employment,” an evidence-based practice in which service providers help a person find and hold a competitive job, is a valuable resource. Yet even people who benefit from this approach may struggle to attain financial self-sufficiency if their jobs are low-paying or part-time, especially if these positions don't qualify them for workplace benefits like health insurance, disability insurance, and paid time off.
Sustainable Employment
While employee readiness is important, there are many other factors that can boost job longevity and success. By prioritizing these alongside employee readiness, we can create the conditions for long-term, sustainable employment. For instance, the potential value of social capital, or “the collective value of social network connections and resources that generate instrumental, informational, and emotional support,” has not yet been fully recognized. Strong social capital increases job satisfaction and retention for everyone — including employees with serious mental health conditions.
Organizational Social Capital
In addition to personal social capital, which includes the support and encouragement of close family, partners, and care providers, the role of organizational social capital is also critical. Organizational social capital refers both to positive social relations with supervisors and coworkers, and to policies and practices that promote healthy workplace norms — features strongly influenced by the culture of each specific workplace. Even an employee with the best job coach in the world can be derailed by an unfriendly or toxic work environment in which they experience discrimination, stigma, unclear expectations, or a murky and difficult process for requesting reasonable accommodations. As these are areas over which employers, not employees, have the most control, organizational leaders who want to help workers with SMHCs to thrive and contribute should consider introducing specific changes in workplace culture.
A Better Workplace for All
So how can employers impact workplace culture to support people with SMHCs? Usually, this shift is facilitated by changes in the areas of onboarding, supervision, and the process for requesting and providing accommodations. Wellness initiatives and SMHC awareness trainings can give all staff good information and tools to meet challenges as they arise, while making the workplace better for everyone. To support these initiatives, employees’ assumptions must be addressed, with leaders taking the important step of directly challenging stereotypes of people with SMHCs as incapable or helpless. Managers will need first to educate themselves, and then to follow up by issuing directives, changing job expectations, offering trainings, and endorsing the efforts of successful supervisors.
People with serious mental health conditions who don’t receive benefits or subsidies need jobs that pay a living wage and that provide crucial workplace benefits. Unfortunately, too many with SMHCs struggle to find and keep such jobs in workplaces unequipped to support their natural resilience. Fortunately, the changes that can lead to sustainable employment for people with SMHCs — such as individualized and regular supervision, efforts to reduce stigma, and efficient approaches to reasonable accommodation — are readily achievable. Furthermore, these shifts are likely to benefit organizations overall.
Future Access blog posts will take a closer look at important elements in sustainable employment. Meantime, find out about TAC's trainings for behavioral health organizations and agencies working with peer specialists.
August 2017: News, Resources, and Happenings at TAC
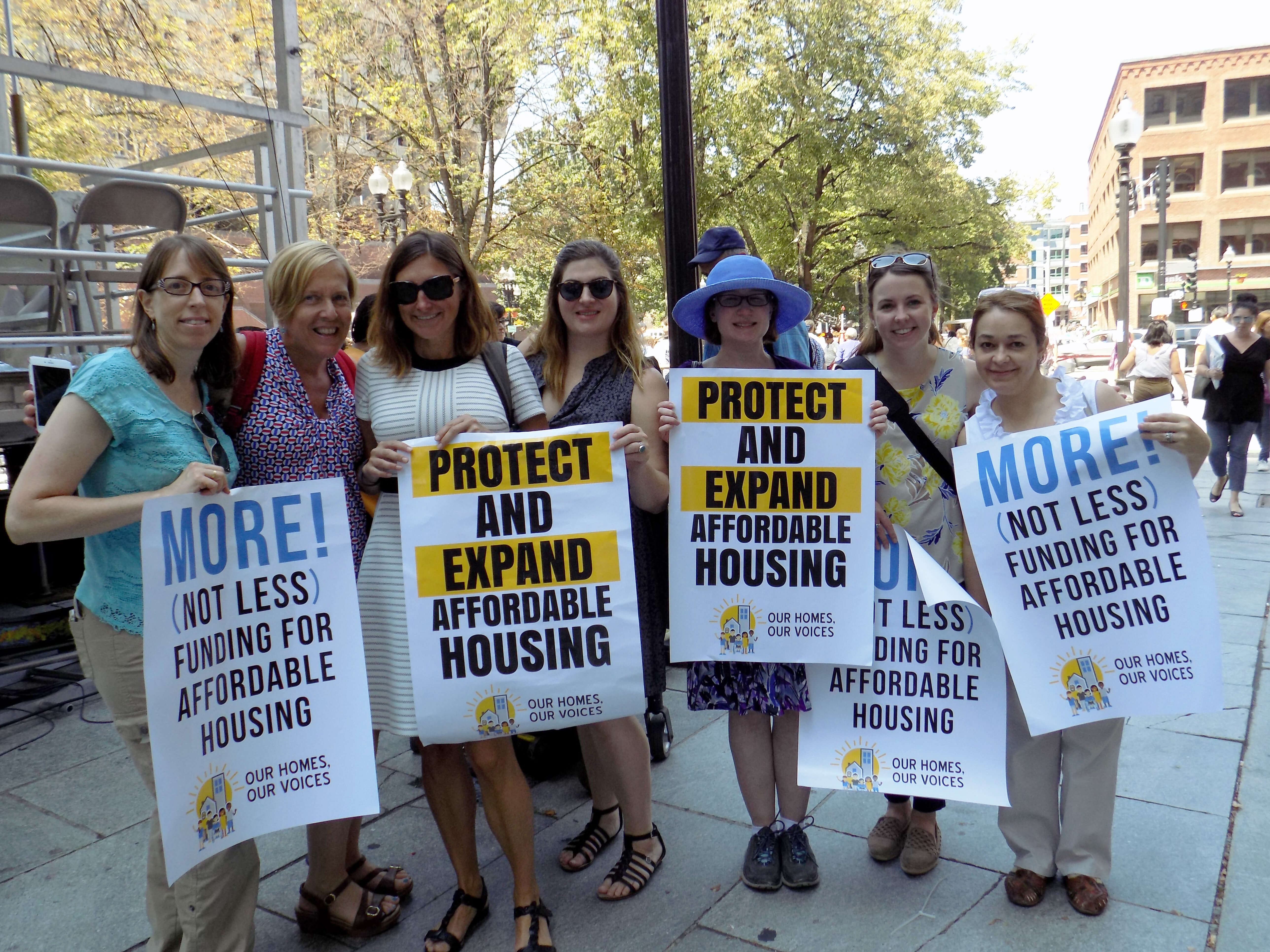
Our Homes, Our Voices — No Housing Cuts!
TAC staff headed over to historic Faneuil Hall a few weeks ago, where we joined hundreds of other housing and disability rights advocates, subsidized housing residents, and community leaders to tell the federal government: NO CUTS TO HOUSING! The Boston rally was organized by our friends at the Citizens' Housing and Planning Association in coordination with events held around the country. Check out our Facebook photo album to see a few of the speakers we cheered for, and take a look at #OurHomesOurVoices on Twitter for a national snapshot.
New Action Plan Launched for Permanent Supportive Housing in North Carolina
Many of the strategies in North Carolina's 2017 Permanent Supportive Housing Action Plan are based on a Permanent Supportive Housing Assessment with Recommendations to Comply with the Olmstead Settlement produced by TAC. The shared vision for permanent supportive housing in North Carolina connects people to affordable, integrated, and supportive housing by leveraging resources and collaborating with all levels of government and private agencies.
CMS Helps States to Foster Community Living Opportunities
The Centers for Medicare and Medicaid Services (CMS) has announced a second round of the State Medicaid-Housing Agency Partnerships track in its Medicaid Innovation Accelerator Program (IAP). The goals of this track are to develop public and private partnerships between state Medicaid and housing systems and to support states in creating detailed action plans that foster community living opportunities for Medicaid beneficiaries. TAC is part of the IAP technical support team that will work from August 2017 through April 2018 with eight states: Alaska, Massachusetts, Michigan, Minnesota, Nebraska, Texas, Utah, and Virginia. Visit the CMS website to learn more.
TAC Staff in Action
STAFF ACTIVITIES
TAC Associates Phillip Allen, Ellen Fitzpatrick, and Ashley Mann-McLellan and Senior Associate Melany Mondello attended the National Conference on Ending Homelessness in Washington, D.C. last month, with presentations by Phil on the SSVF System Assessment Toolkit and by Ashley on the intersection of housing, mental health, and substance abuse; Jon Delman, Senior Associate, was an invited participant in SAMHSA's expert resource meeting on "Advancing Behavioral Health Treatment & Recovery through Technology" and led a workshop on "Fighting for our Livelihoods: Developing Job Opportunities for Economic Self-Sufficiency" at the National Empowerment Center's Alternatives Conference; Associate Lauren Knott and other experts helped out at a forum for SAMHSA's 10 Youth Homelessness Demonstration communities; Executive Director Kevin Martone described the importance of affordable housing for people with disabilities at a #NoHousingCuts Congressional reception organized by Monarch Housing Associates of New Jersey; Kevin also spoke on the role of community-based mental health services and housing in reducing reliance on emergency and inpatient care in his address to mental health authority leaders gathered at the National Association of State Mental Health Program Directors' annual conference; and Senior Consultant Jim Yates was promoted to the rank of Colonel in the Army National Guard - congratulations, Jim!
STAFF TRANSITIONS
We are happy to welcome Hawo Osman as a TAC intern this summer. Hawo is a rising senior at Medford High school and joins us through the Boston Center for Independent Living’s Transition Internship Program.
July 2017: News, Resources, and Happenings at TAC
TAC Scholarship Helps Launch a Teacher, a Social Worker, a Nurse, and a Chef
We are delighted to introduce this year’s recipients of the second annual Day-O'Hara Community Integration Scholarship. This cash award, given in honor of TAC co-founders Steve Day and Ann O'Hara, is intended to help individuals with disabilities in the Greater Boston area to realize their educational and professional goals.
Eddie Shields is currently employed as a teacher’s assistant and was referred to us through the Boston Center for Independent Living. He will use the scholarship money towards courses to obtain his Associate’s Degree in early childhood education.
Kayla Wilson is a Long-term Support Services Coordinator at the Boston Center for Independent Living. Kayla has discovered that her true passion is to assist individuals from both the medical and social points of view simultaneously, and plans to use the scholarship money towards prerequisite courses for nursing programs.
For two years, Lisa Jones has volunteered weekly to serve meals to elders in need. Lisa was referred to us by the Transformation Center, and will use the scholarship money for a post-bachelors program in gerontology — moving her closer to her goal of attaining a Master’s degree in social work or human services so that she can work in a wraparound program to help elders stay in their own homes.
Silvaria DeSilva has a background in nursing, but has recently discovered a love for cooking. She recently graduated from Pine Street Inn’s food service training program, and will use the scholarship money for cooking classes and to buy the supplies and materials she’ll need as a professional chef or caterer.
Best of luck to all, and thanks to the partner organizations that helped us connect with these inspiring individuals!
Successfully Employing and Financing Peer Specialists in Behavioral Health
The inclusion of peer providers on behavioral health care teams can significantly improve client engagement and outcomes, including symptom reduction, improved self-esteem, and community integration. Yet behavioral health providers sometimes struggle to maintain a strong peer workforce — leading to diminished productivity and increased stress for all staff. In TAC’s new training for behavioral health providers, managed care organizations, and state/county behavioral health authorities, participants will learn how to introduce appropriate supports and key shifts in workplace culture to promote both peer job success and stronger organizations overall.
TAC Staff in Action
Staff Activities
In June, Managing Director Marie Herb and Senior Associate Gina Schaak served as volunteer “Ambassadors” at Boston’s Third Surge to End Chronic Homelessness (read all about it!); TAC Associate Ashley Mann-McLellan presented on “Using Data to Improve Outcomes and HUD’s System Performance Measures” at the All Home Annual Conference in Seattle, WA; Kevin Martone, Executive Director, recorded a webinar for Foothold Technology on "Navigating the World of Medicaid for Supportive Housing Services"; and at the National Coalition for Homeless Veterans conference, TAC Associate Douglas Tetrault co-presented with our partners from Abt Associates on how to assess the components of a crisis response system and develop improvement strategies.
June 2017: News, Resources, and Happenings at TAC
Propelling Innovation to End Youth Homelessness
TAC consultants have been criss-crossing the U.S. this spring to help strengthen local youth homelessness prevention efforts. In Washington's Seattle/King County, our TA is an integral part of the Youth Homelessness Demonstration Program, a HUD initiative awarded to ten communities. So far, we've worked with Seattle/King County on flexible system design, engaging a Youth Advisory Board, compiling promising practices from across the country, analyzing data to measure the need for housing and services, creating landscape scans of current housing and service inventories, and developing continuous improvement strategies the community can use to evaluate and learn from implementation. Once the planning process wraps up in July, our focus will shift to creating an implementation "road map" for community stakeholders and providing training and capacity-building to Seattle/King County agencies working to end youth homelessness in their community. Learn more about TAC's TA with programs serving children and youth.
Sharing Strategies for Successful Community Integration
From May 1-2, HUD Section 811 Project Rental Assistance grantees from 25 states — including both housing and service providers — joined TAC staff members and officials from the Department of Housing and Urban Development (HUD) and the Centers for Medicare and Medicaid Services (CMS) in Washington, DC. Participants in this TAC-organized initiative shared successes and insights from their experiences implementing PRA to expand integrated supportive housing opportunities for extremely low-income people with disabilities.
TAC Staff in Action
STAFF ACTIVITIES
Policy Advisor Francine Arienti and TAC consultant Naomi Sweitzer were invited by the Vermont Youth Homelessness Prevention Plan Committee to present on federal/state resources and models of state plans around the country; Senior Associate Jonathan Delman gave the keynote address at Employment Matters! (annual conference of the Massachusetts Association of People Supporting Employment First); Jon's article on "Employer-based Strategies to Increase Employment Rates for People Living with Serious Mental Illness," co-authored with Senior Consultant Lynn Kovich and Executive Director Kevin Martone, has been published in Psychiatric Rehabilitation Journal; Associate Ashley Mann-McLellan hosted a community planning meeting in Denver to help advance the city's strategy on ending veteran homelessness; Ashley also met with HUD Youth Homelessness Demonstration Project grantees and TA providers at the CSH Supportive Housing Summit in May; and Associate Douglas Tetrault presented on "Community-wide System Assessment and Improvement" at the National Coalition for Homeless Veterans conference, while Senior Consultant Jim Yates presented on "Using Federal Fair Housing Guidance to Reduce Access Barriers to Housing" at NCHV's pre-conference Housing Summit.
POSITION AVAILABLE
TAC is seeking a Senior Associate/Consultant with expertise in behavioral health and Medicaid. Read the full description and application information.
March 2017: Two Olmstead Settlement Agreements Resolved, but the Future of Community Integration is Unclear
DEPENDING ON WHOM YOU ASK, an Olmstead settlement agreement can be a blessing or a curse. While the parties typically agree on the principle affirmed by the U.S. Supreme Court — that people with disabilities should live in the most integrated setting possible — costly housing markets and complex service delivery systems are formidable barriers to this goal. More than 15 years after the Supreme Court's landmark Olmstead decision, states still struggle to serve people with disabilities in integrated settings.
Delaware and New Jersey are two states that have recently resolved their Olmstead settlements, achieving significant reforms though years of dedicated effort — Delaware's settlement was originally signed in 2011 with the U.S. Department of Justice, while New Jersey's was signed in 2009 with Disability Rights New Jersey and the Bazelon Center for Mental Health Law.
Thanks to the successes of these states in substantially attaining the outcomes required by their agreements, thousands of people with serious mental illness now have the opportunity to live in integrated community settings. What is perhaps most impressive is that a substantial part of the system reform accomplished by New Jersey and Delaware occurred during the great recession (2007 to 2009) and the following period of slow economic recovery.
Getting Results
Delaware and New Jersey both offer good examples of what is possible when states focus on community integration for people with mental illness and other disabilities.
A U.S. Department of Justice press release describes some of Delaware’s most significant gains. The state reduced the number of bed days in the Delaware Psychiatric Center by 47.2 percent. The number of Medicaid-eligible Delawareans receiving community-based services has increased by 92 percent since the United States began its investigation. The state has seen the growth of a strong peer and self-advocacy movement that is now incorporated into its entire service system. Two statewide mobile crisis teams and a crisis walk-in center divert 70 to 90 percent of the individuals they engage away from hospitalization and criminal justice interaction and toward community-based services.
As a press release from Bazelon details, New Jersey’s settlement also brought about important changes. Between 2005 and 2016, New Jersey invested nearly $104 million in services and rental assistance for Olmstead-related activities. The state also established a $200 million special needs housing trust fund, and created nearly 1,500 new permanent supportive housing units through capital and rental assistance. New Jersey’s state psychiatric hospital census was reduced by a third, patients’ average length of stay went down, and one state hospital was closed — changes that allowed state hospital operating funds to be reinvested in community supports. New Jersey created a Medicaid benefit to fund community support services for residents of supportive housing, and leveraged additional Medicaid money with investments in community-based services.
Both Delaware and New Jersey used their Olmstead settlement agreements as a driver for change, embracing a community integration platform to guide them toward significant behavioral health system reform. These states recognized that without sustainable system reform and new resources, counting numbers to achieve settlement targets wouldn’t bring about the changes needed to serve people with serious mental illness effectively.
Commitment to Olmstead in a Changing Landscape
Across the country, Olmstead stakeholders are raising questions about the future of community integration for people with serious mental illness and other disabilities. Doubt surrounds the capacity and motivation of states to tackle Olmstead in the years ahead; the commitment of the Department of Justice to focus on Olmstead as strongly as it has in the past; and the ability of protection and advocacy organizations to hold states accountable.
Changes to the Medicaid landscape at the federal level could put at risk the types of benefits coverage that makes community integration work for people with disabilities. Looming cuts to non-mandatory discretionary budgets, such as HUD housing assistance programs, may further jeopardize the ability of states to support community integration.
The Department of Justice has been instrumental in the movement toward community integration, enforcing Olmstead by leading investigations, entering into settlement agreements in several states, and intervening in support of class actions. If the Department shifts its attention to other priorities established by the Trump administration, individuals with serious mental illness and other disabilities will be left without civil rights enforcement at the very time when loss of benefits could place them at greater risk of institutionalization. Many state protection and advocacy agencies, as well as legal services organizations, have the authority to bring class action lawsuits on behalf of people with disabilities, and these groups may be called upon to step up their efforts.
Complying with Olmstead will become increasingly difficult if federal policy and budgetary changes reduce support to states in the near future. Federal cuts currently under consideration would put people with mental illness and other disabilities at greater risk of institutionalization and homelessness due to thinner benefits and services and reductions to the rental assistance that can make housing affordable. Our February blog post on budget impacts explained the challenges states will face in making resources available to meet federal requirements. Nevertheless, it is states that are on the hook to ensure that individuals are served in integrated settings.
Community integration mandates in the Olmstead decision, Title II of the Americans with Disabilities Act, and Section 504 of the Rehabilitation Act are still the law, regardless of fluctuations in federal enforcement and support. Furthermore, serving individuals with disabilities in integrated, community-based settings is good, cost-effective policy. With these facts in mind, states should continue to design and implement Olmstead plans that build sustainable, system-wide improvements. The benefits — to individuals, communities, and all who recognize the value of true integration — are well worth the challenges.
News, Resources, & Happenings at TAC: February 2017
Core Principles for Housing and Health Care Policy: A Statement from TAC
TAC's Board of Directors met on December 8, 2016, to discuss the ways our organization can help ensure that leaders make informed decisions about proposed changes to health care and insurance, affordable housing, social and economic policies, and the other programs that form our country's safety net. On January 10, we issued a statement of the principles that will guide our work and advocacy in the months and years ahead.
Read the full statement.
Educating Congress on the Important Role of Medicaid in Preventing and Treating Substance Abuse Disorders
On January 25, TAC Director Kevin Martone and other panelists addressed some 70 congressional staffers representing legislators of both parties. Organized in partnership with the National Council for Behavioral Health, this event offered lawmakers the opportunity to learn that decreased federal support would have a devastating effect on state substance use treatment systems - and showed them why preservation of coverage for individuals with substance use disorders is crucial.
Melville Charitable Trust Roundtable Highlights Housing Program Progress
Since 2012, HUD has awarded Section 811 Project-based Rental Assistance (PRA) funds to 28 states and the District of Columbia. By establishing state-level partnerships among housing, Medicaid, and human services agencies, these state grantees have been able to develop integrated, affordable, accessible housing opportunities - with access to voluntary supports - for people with disabilities who have extremely low incomes. Under contract with the Department of Housing and Urban Development (HUD), TAC is a provider of TA for these Section 811 PRA grantees. On January 12, TAC facilitated a Melville Charitable Trust-sponsored roundtable event to discuss the demonstration program's progress. The roundtable included participants from six states (MN, NJ, PA, MD, TX, and LA), HUD staff, the National Council of State Housing Agencies, the National Low Income Housing Coalition, and the Center on Budget and Policy Priorities. A lively discussion focused on recommendations to increase access to affordable housing, leverage resources effectively, and identify best practices in service delivery.
TAC Staff in Action
Staff Activities
Associate Ashley Mann-McLellan recently led a workshop for funders in Seattle/King County, WA on how to incorporate Housing First principles into their requirements, contracts, and monitoring processes - and, together with Associate Lauren Knott, conducted a Housing First training for the Cambridge (MA) Continuum of Care;Working with the Supportive Services for Veteran Families (SSVF) program and the U.S. Interagency Council on Homelessness, TAC Associate Doug Tetrault helped plan and facilitate a community meeting for 60 local stakeholders focused on effectively ending veteran homelessness in Orlando, FL; Senior Associate Jon Delman's symposium on "Successfully Employing Young Adult Peer Mentors: From Research to Practice with the Employer Toolkit" has been accepted by the Psychiatric Rehabilitation Association for its 40th annual Wellness and Recovery Summit; Kevin Martone, TAC's Executive Director, spoke at a Congressional briefing this month on "Expanding Access to Care," hosted by the National Council for Behavioral Health; Kevin also spoke at the National Press Club on December 12 as part of the National Governors' Association event "Housing as Health Care: A Roadmap for States"; and in December, Senior Policy Advisor Lisa Sloane presented on Louisiana's Section 811 PRA program at a public workshop hosted by the National Academies of Sciences, Engineering, and Medicine; and Associate Amy Horton and Senior Associate Gina Schaak volunteered at Boston's Homeless Count the night of January 25.
TAC Transitions
Congratulations to Liz Stewart on her promotion to Senior Associate with the TAC housing team!